How to Develop a HIPAA-Compliant App: A Complete Guide
The healthcare industry in the United States is a somewhat complicated area. There are many health insurance plans (private health insurance for the majority and public health insurance for low-income people and the disabled), many providers, and many diverse payments coming from numerous payers.
The complexity of this multi-layer system, in turn, makes it pretty hard to govern, control, and protect every single part of it. That is why many sources are increasingly reporting various leaks of confidential data.
Between January and September 2024, US healthcare organizations suffered 491 major data breaches with over 500 records compromised. Hereby, the figure has risen over the last ten years.
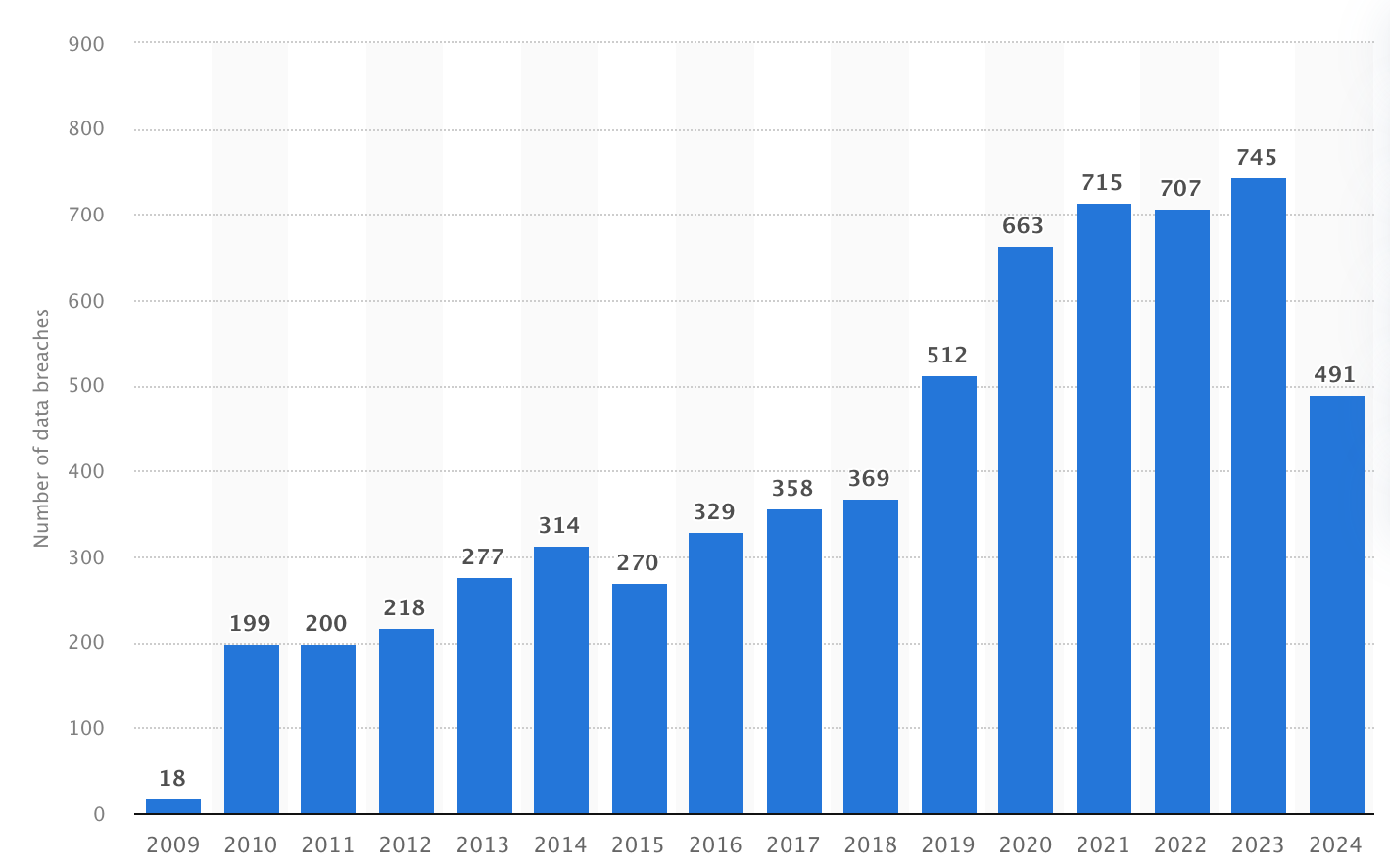
Number of healthcare data breaches in the United States (2009-2024), Statista
To prevent any degree of information leakage, all medical apps in the US are obliged to follow HIPAA regulations (Health Insurance Portability and Accountability Act).
In this guide, we’ll walk you through everything you need to know about HIPAA-compliant app development—from essential certifications and software development stages to common mistakes, costs, and future trends.
What is HIPAA and Why Does It Matter?
Essentially, HIPAA is a federal American regulation whose objective is to protect patient health information (PHI). It sets standards for the storage, transmission, and access of healthcare information to avoid breaches and unwanted access.
Many healthcare organizations rely on electronic health records (EHR) as the core systems for managing patient information, making their proper protection under HIPAA regulations especially important.
For medical establishments that plunge into health app development services, HIPAA compliance is not only a legal matter—it’s a commitment to establish trust, avoid hefty fines, and protect data.
Non-compliance and HIPAA violations can mean monetary penalties of thousands to millions of dollars, in addition to damaging reputation.

Amount of fines for HIPAA violations (August 2024), Statista
Key HIPAA Rules and Their Impact on App Development
The HIPAA law was passed in 1996 in order to make the healthcare system more adequate and prompt. The legislators were aware that electronic systems have the chance to expose patients’ private health information.
Therefore, HIPAA was split into several separate regulations that altogether must protect individuals’ personal health information or mitigate the consequences of breaches.
- The Privacy Rule: The Privacy Rule creates standards for the use and disclosure of health information. It protects people’s private health records and gives them the right to find out about the use of their information. The rule applies to certain organizations, including hospitals, doctors, and insurance companies, which are known as “covered entities.”
- The Security Rule: The HIPAA Security Rule executes standards for safeguarding electronic health data. It regulates any organization that collects or processes this kind of information from corresponding software, e.g., wellness or doctor apps. The rule requires them to have adequate protections in place—decent policies, safe systems, and safe storage on physical devices.
- Breach Reporting: If there’s a data breach, HIPAA Breach Reporting mandates the app provider to inform users, the Department of Health and Human Services (HHS), and sometimes the media.
- The Enforcement Rule: The HIPAA Enforcement Rule encompasses compliance and investigation provisions, evaluation of civil money penalties for violating the HIPAA Administrative Simplification Rule, as well as procedures for hearing.
Must-Have Features in a HIPAA-Compliant Software
When you make a healthcare app that holds confidential patient data, HIPAA compliance is mandatory. But being compliant isn’t so much about checking boxes as it is about putting certain features in place that safeguard personal health details.

First, your mobile app calls for data encryption. This means all health data must be encrypted to unreadable form when it’s being stored or transmitted. Therefore even if someone steals the data, they will not be able to read it.
Then make sure you have resilient user authentication, which means only authenticated people (doctors, nurses, or patients) should be able to log in and see specific information. This can be via passwords, two-factor authentication (e.g., a code texted to your phone), or even face ID or fingerprint.
Besides, you would have to enforce role-based access control. Not everybody needs to be able to view everything.
For example, a physician will need to view medical records, but a receptionist will only need to view appointment data. Role-based control minimizes access to an absolute minimum of what is necessary.
Additionally, include automatic log-out. If a person forgets to log out of the mobile app, it should log them out after a short period of inactivity to prevent other individuals from inadvertently accessing confidential records.
If your application provides messaging, video calling, or sharing files, all of those components must also be unassailable. All communication has to be made secure so that no one outside the application can listen in or see private documents.
And just in case things do go amiss, your app should have a breach notification attribute. It needs to be capable of detecting the problem and notifying users and proper authorities quickly, as HIPAA requires.
Finally, bear in mind that it is an ongoing job to remain safe. When you develop HIPAA-compliant mobile software, your app must have space for regular updates and security fixes to defend against new dangers as they are identified.
Steps to Build a HIPAA-Compliant Mobile App
In 2023, it was reported that 35% of US businesses that export data abroad said privacy regulations are an added cost. Additionally, 17% said regulations were a notable barrier to cross-border trade.
Yet, the absence of a general data privacy protection law on the federal front makes any company conflicting with other states or regions that have more uncompromising commitments.
Thus, HIPAA-compliant mobile app development services (no matter whether iOS or Android) must be structured into a process that includes not only writing the code, but also building trust, protecting health data, and adhering to strict regulations at every step.
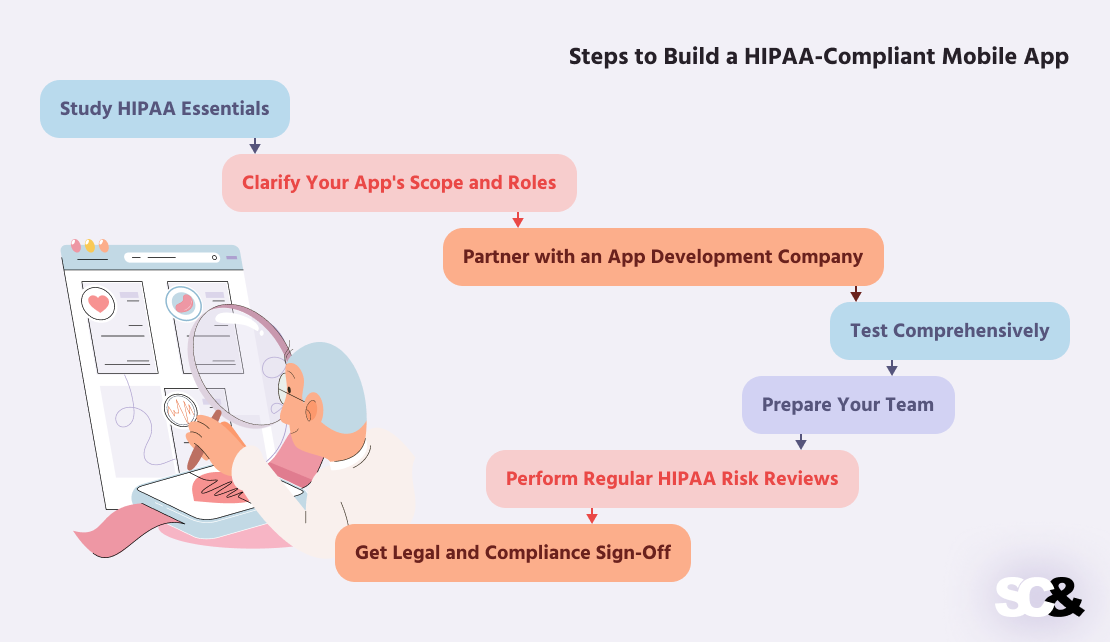
1. Study HIPAA Essentials
Before writing a single line of code, start by getting yourself acquainted with what HIPAA requires in general. You need to know what kind of data constitutes protected health information, what decrees cover the storage and disclosure of that information, and what technical, physical, and administrative precautions are mandated.
2. Clarify Your App’s Scope and Roles
Second, explicitly state what your healthcare application will do, who will use it (patients, physicians, employees, etc.), and what type of health data it will control. At this point, decide whether your app is a “covered entity” or a “business associate” because HIPAA directions are slightly different for each.
3. Partner with an App Development Company
One of the smartest moves you can make when you dive into HIPAA-compliant app development is to partner with an application development team, such as SCAND, that has expertise in the subtleties of healthcare software development.
A good partner will help you select the right mobile app development approach, choose a tech stack for different mobile devices, and take care of implementing all the required security features, including encryption, user authentication, audit logs, and automatic logouts.
They’ll also make sure your app includes appropriate role-based access control, so users only see the information they actually need.
4. Test Comprehensively
Compliance and security testing go hand in hand when making software. Beyond functional tests, it’s important to test for vulnerabilities, encryption weaknesses, misconfigured access controls, and logging problems. If feasible, hire external security professionals to review your app.
5. Prepare Your Team
Make sure everyone involved, from app developers to support staff, understands HIPAA basics. Training is a part of compliance. Even a great app can be made non-compliant when patient information is mishandled by someone who is not aware.
6. Perform Regular HIPAA Risk Reviews
Perform a risk analysis before launching your app (and regularly afterward). This will uncover any spots where your app’s security, data handling, or infrastructure could be at risk.
7. Get Legal and Compliance Sign-Off
Have legal and compliance professionals review your app and documentation prior to going live. They can guarantee that your app is HIPAA compliant in all respects and help with the last-minute details, such as signing Business Associate Agreements (BAA) with any third-party vendors that you use.
8. Watch, Update, and Stay Compliant
HIPAA compliance is not a one-off activity—it’s continuous. After going live, continue to watch your app for exposures, regularly revise it, and perform periodic audits to keep yourself in compliance with all of the provisions as laws and technology change.
Common Mistakes in HIPAA Compliance and How to Avoid Them
It is difficult to develop a HIPAA-compliant app when even minor mistakes can cause serious problems, such as data breaches or legal ramifications. The bright side is that most of them can be bypassed if you know what to look for.
One of the most common mistakes is not knowing what protected health information is. PHI isn’t merely medical records—it’s any individual information related to a person’s wellness. If you don’t protect this type of information adequately, you could unknowingly violate HIPAA guidelines.
Another common mistake is skipping the risk assessment (you can find more about it below). Before you launch your app, you need to check for potential protection threats.
Many developers either forget this step or put it off. But if you don’t assess your app’s security, you can’t know if there are defects that need correcting.
Choosing the incorrect services and tools is a frequent mistake too. Not all cloud services or tools are HIPAA-compliant. If you use a service that will not execute a BAA, it is not safe to use for the processing of PHI.
| Common Mistakes | Why It’s a Problem | How to Avoid It |
| Not understanding what PHI includes | You may accidentally expose or mishandle protected data without realizing it. | Learn what qualifies as PHI—it’s not just medical records but any health-related data. |
| Skipping the risk assessment | Security flaws go undetected, increasing the chance of data breaches. | Always perform a thorough HIPAA risk assessment before launch. |
| Delaying the risk assessment | Postponing it means you might miss vulnerabilities during critical stages of dev. | Make it part of your early and ongoing development process. |
| Using non-compliant tools or cloud services | Using platforms that won’t sign a BAA can result in non-compliance and data exposure. | Choose vendors and tools that explicitly support HIPAA and provide BAAs. |
How to Conduct a HIPAA Risk Assessment
A HIPAA risk assessment is important for ensuring that your app stays compliant and protects sensitive health data. It might seem complicated at first, but if you break it down into steps, it becomes much easier to handle.
First, you need to understand exactly what type of health data your app handles. Include not just medical records, but also personal information like:
- Names
- Phone numbers
- Insurance details
- Appointment dates
Knowing what data you’re collecting, storing, or sharing helps you figure out what needs to be protected.
Next, you need to determine who has access to that data, such as your team, patients and healthcare providers, or third-party vendors. Not everyone should have full access to all the data, so it’s important to set up access controls that allow users to see only the information they need.
Once you know what data you have and who can access it, you should look at your current security measures. Are you using encryption, secure logins, and proper access control to protect the data?
You also need to consider physical security, like how and where you store the data. If there are any gaps in your security, you’ll need to address them to stay compliant with HIPAA.
Then, you need to think about the potential risks to the data. These could come from internal mistakes, like an employee accidentally exposing information, or external threats, like hacking attempts. By identifying these risks, you can figure out what parts of your app might be vulnerable and what needs to be improved.
After that, evaluate the impact of these risks. How bad would it be if a breach happened? Would sensitive data be exposed? How likely is it that this might happen? This helps you prioritize which risks need to be dealt with first.
When you’ve figured out the risks, it’s time to take action. You might need to strengthen your encryption, improve login security, limit who has access to certain data, or conduct regular security checks.
It’s also important to document everything you do during the risk assessment. Keep track of what data you handle, the risks you’ve found, the security measures you’ve put in place, and any changes you make. This is important for HIPAA compliance and will help you during audits or if any issues arise in the future.
Finally, remember that HIPAA compliance isn’t something you do just once. As your app changes and new threats emerge, you need to regularly review and update your risk assessment. This way, you can keep your app compliant and ensure the data stays safe.
How to Get a HIPAA Compliance Certification
HIPAA certification is verified by HIPAA training to validate the understanding of corresponding compliance necessities, normally done annually. Successful trainees are awarded a HIPAA compliance certificate.

For a company, HIPAA certification is when a third-party verifier confirms whether the company abides by all the regulations needed to protect health information.
Having a HIPAA certificate of compliance is a large part of proving that your app or business is entirely secure, and there are some things you can do to prove you’re HIPAA compliant:
- Become familiar with HIPAA’s Privacy, Security, and Breach Notification Rules that contain guidelines to protect PHI.
- Carry out an assessment for specifying potential gaps for governing PHI.
- Develop and put in place administrative, physical, and technical safeguards to manage recognized risks.
- Educate staff on HIPAA policies and procedures relevant to their roles to deal with PHI in the appropriate manner.
- Hire an independent company to inspect your compliance measures via audits and appraisals.
- Enforce corrective actions on the basis of audit findings to shut any compliance gaps.
- On successful compliance, obtain a formal certification of adhering to HIPAA standards.
Although there is no HIPAA certification issued by the government, you can work with a trustworthy third-party auditor. These experts will audit your systems and check if they are HIPAA compliant.
If you meet their audit, they will give you a report or certificate stating you are compliant, something that is very important for showing clients and partners that you are following the regulations.
Cost of HIPAA Compliance
HIPAA compliance can be from extremely affordable to extremely costly, depending upon the size and complexity of your organization or app. There is no fixed cost to become compliant, but having an idea of where the costs most often lie, you can budget accordingly and not be caught off guard.

First, you need to consider the costs associated with implementing the necessary security measures:
- Data encryption
- Access control systems
- Secure login protocols
- Audit logging software
- Secure cloud hosting services (with signed BAAs)
Depending on the technologies involved, these software solutions can be expensive to deploy, especially for small businesses. Spending on good security, however, is the price you must pay for protecting sensitive health information and achieving compliance.
Then, there’s the expense of paying professionals to do a proper risk assessment and audit your systems. Risk assessment is an important aspect of HIPAA compliance that checks for weaknesses and improvements needed.
Most companies opt to hire third-party auditors or security consultants, who generally charge by the hour or have a flat rate. Fees vary but can range from:
- $1,000 to $5,000 for small-size assessments
- $10,000 or more for large-scale systems or enterprise apps
Also on the list is training your employees. Since HIPAA requires all employees to be aware of how to handle the protected health information correctly, you’ll need to invest in training sessions. These expenses generally include:
- Drawing up or buying training materials
- Paying for access to online courses or certification tools
- Giving time for staff to attend training sessions
Another part to consider is the cost of recurring monitoring and auditing. When you have obtained compliance, you must maintain your systems up to date. This involves:
- Inside or outside safety audits
- Successive exposure scanning
- Monitoring tools to detect and react to possible breaches
Though these expenses fluctuate, regular inspections are necessary to remain in compliance and avoid fines.
Finally, don’t neglect legal services. You may have to work with lawyers to develop or negotiate Business Associate Agreements (BAAs), and privacy policies, or address breaches. Legal fees could include:
- Consultation fees for HIPAA-related legal questions
- Reviewing and updating contracts with vendors
- Assistance in case of a data breach or compliance issue
By and large, HIPAA compliance costs generally fall within the following five categories: implementation of security, risk analyses, training of personnel, ongoing monitoring, and legal fees.
Despite the fact that the overall expense might seem high, the investment is necessary to safeguard patient records, avoid penalties, and gain the trust of users.
Successful HIPAA-Compliant Apps You Can Refer to When Developing Your Software
To better understand what it takes to make an app that adheres to HIPAA, let’s take a look at some examples of apps that successfully comply with HIPAA requirements.

These cases illustrate how different companies have navigated different challenges in compliance and what things you can refer to when collecting requirements for your own application.
Teladoc Health
Teladoc is a top US telemedicine platform with millions of virtual healthcare users. Since the platform holds personal medical information during video consultations, messages, and drug issuance, compliance with HIPAA is non-negotiable.
To remain compliant, Teladoc:
- Uses end-to-end encryption for all communication between providers and patients
- Enforces multi-factor authentication to secure user access
- Has strict access controls and audits all interactions involving PHI
Overall, Teladoc’s achievement is proof that no matter the size, a medical platform can remain protected and convenient to use with HIPAA mandates put at the core of its infrastructure and design.
MyChart by Epic Systems
MyChart is a patient portal that allows users to review lab tests, schedule appointments, send messages to doctors, and manage medications. When interacting directly with clinics, hospitals, and other healthcare organizations, HIPAA compliance is a must.
Fundamental HIPAA-priority features on MyChart include:
- Role-based access that limits what data different users (patients, physicians, admins) are allowed to see
- HIPAA-compliant secure messaging that meets HIPAA’s privacy and security requirements
- Strong audit trails that help track access to PHI
Epic’s approach demonstrates how health apps can be embedded with clinical systems while still having strong data privacy.
Doxy.me
Doxy.me is a telemedicine video conferencing software of choice for small practices and solo providers. Unlike larger enterprise-level systems, Doxy.me does not compromise user experience to become fully HIPAA compliant.
They accomplish this by:
- Offering BAAs to all paid plan users
- Hosting all data on HIPAA-compliant infrastructure
- Peer-to-peer video calls that are encrypted and don’t store PHI
In general, Doxy.me shows that even simple applications can achieve compliance needs without over-complicating the user interface.
Future Trends in HIPAA Compliance and Healthcare App Development
As healthcare apps keep pushing the boundaries with artificial intelligence and remote patient monitoring, data security will be more consequential than ever before.
First, privacy and security will have to be prioritized by developers from the very beginning of the development process. This will mean producing software that is equipped with strong encryption, authentication, and clear user permissions from the inception.
More health apps will also be submitted to third-party audits in the future to comply with HIPAA. Cloud providers will offer more services and tools specifically designed to be HIPAA compliant.
At the same time, as healthcare systems become more dependent on sharing data, developers will need to prove that data is transmitted back and forth securely and accessed by only approved individuals.
In other words, successfully creating healthcare apps will mean that developers will need to stay on top of new technology and never let their guard down in regard to protecting patient privacy and data.
Frequently Asked Questions (FAQs)
What applications need HIPAA compliance?
Any app that handles PHI and is used by healthcare providers, payers, or business associates must be HIPAA compliant. Telemedicine apps, EHR solutions, and medical billing apps come under this umbrella.
How much does HIPAA-compliant development cost?
Pricing varies but is usually between $50,000 and $500,000 based on security requirements, integrations, and compliance auditing.
How often should an application be audited for HIPAA compliance?
Routine audits ought to be undertaken at least yearly, with added evaluations when noteworthy updates or security modifications are applied.












